Abstract
Introduction: Multiple Myeloma (MM) is the paradigm of a tumor in its microenvironment and usually MM cells are highly dependent on the bone marrow niche. However, a group of patients with poor prognosis present with extramedullary disease (EMD), which refers to growth of malignant plasma cell tumors outside the bone marrow not being adjacent to bone. EMD is an aggressive form of MM that is associated with high-risk genomic aberrations, increased proliferation, and poor survival. Even in the era of highly active, T-cell based treatments such as Ciltacabtagene autoleucel, EMD remains difficult to treat, highlighting an ongoing need for improved understanding of the biology underlying this condition.
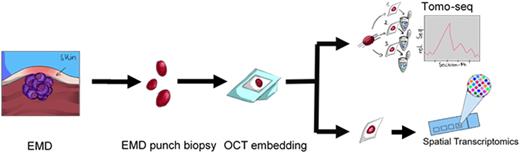
Recently, novel technologies unraveled a complex spatial architecture of solid tumors highlighted by multicellular niches that support tumor growth or prevent immune cell infiltration and subsequent anti-tumor immunity. Whether these observations hold true for EMD is unknown, but a common notion was that EMD solely consist of plasma cells (PCs). Thus, we sought to investigate the EMD microenvironment in a spatial context using Tomo-seq and spatial transcriptomics.
Methods: Tomo-seq is bulk mRNA-sequencing of consecutive sections of frozen tissue with the aim of compiling spatial information and genome wide expression of an entire tumor (Figure 1). We used Tomo-seq to analyze 1 x 2 cm sized extramedullary lump resected from a skin lesion of 84 years old male patient. Furthermore, we performed 10x Visium spatial gene expression analysis on 10 µm sections from 3 male (Age: 84, 61, 70 years) and 3 female (Age: 65,54,77) patients (Figure 1), including 2 patients who relapsed with EMD after either anti-BCMA CAR T or bispecific antibodies. After sequencing and preprocessing, data were mapped to human reference genome (GRCh38) and finally analysis was conducted using Tomoda for the Tomo-seq and Giotto for Visium.
Results: Tomo-seq on 43 30-µm-consecutive sections of a complete EMD lesion revealed that EMD is not solely composed of PCs. PCs constituted 44-55% of the lesion whereas CD8 T cells, blood endothelial cells, macrophages and muscle cells shared the rest. We further comprehensively explored gene-expression profiles by conducting pathway enrichment analysis based on the upregulated genes in each section (z score threshold >= 2). Significant pathways related to angiogenesis, extracellular matrix, cell cycle, cell adhesion and others were upregulated in distinct sections of the EMD tumor. Together, we identified intratumor heterogeneity in EMD.
We moved on and analyzed 6 EMD samples using the Visium spatial transcriptomics to spatially investigate EMD lesions at near single-cell resolution. In our combined analysis, we observed profound interpatient and intratumor heterogeneity. Here, the Visium data robustly reflected the Tomo-seq, with PCs being the primary cell type in EMD. Based on genes implicated in metabolic activity, PCs differed significantly within the same tumor, and the same holds true for genes encoding immunotherapy targets such as SLAMF7 or BCMA. Several immune cell types such as T cells, macrophages, dendritic cells, and NK cells infiltrated the lesions. The gross picture was in line with a poorly organized and even chaotic tumor architecture in EMD. Intriguingly, in some patients, T-cell infiltration was not homogeneous but rather nodule-forming, suggesting focal accumulation of immune cells for reasons, which have yet to be elucidated. In most patients, T cells expressed exhaustion marker genes such as LAG3 and CTLA4. We also detected a T-cell signature in one patient who relapsed with numerous EMD lesions 5 months after CAR T-cell therapy. Flow cytometry from the same lesion revealed presence of BCMA CAR T-cells, and their numbers were significantly increased when compared to CAR T-cell frequencies in peripheral blood assessed at the same time point. Thus, there was an intralesional enrichment of CAR T-cells, but the patient still relapsed, suggesting functional CAR T-cells deficits rather than an infiltration issue in this case.
Conclusion: Using state-of-the-art spatial techniques, we show that EMD is more than just sheets of PCs. We identified immune cells, fibroblasts, and blood endothelial cells or even CAR T-cells contributing to the microenvironment, highlighting a multicellular ecosystem in extramedullary lesions of MM.
Disclosures
Duell:Regeneron: Research Funding; Incyte: Consultancy; MorphoSys: Consultancy, Research Funding. Einsele:BMS/Celgene: Consultancy, Membership on an entity's Board of Directors or advisory committees, Other: Travel Grants, Research Funding; Janssen: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Travel Grants, Research Funding; Amgen: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: travel grants; Takeda: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: travel grants; Sanofi: Consultancy, Honoraria, Research Funding; GSK: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis: Other: travel grants. Rasche:GSK: Honoraria; Pfizer: Honoraria, Membership on an entity's Board of Directors or advisory committees; Sanofi: Honoraria, Membership on an entity's Board of Directors or advisory committees; Janssen: Honoraria, Membership on an entity's Board of Directors or advisory committees; BMS: Honoraria, Membership on an entity's Board of Directors or advisory committees; Amgen: Honoraria, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal